
Once you experience the Zen Timepiece's progressive tones, you'll never want to meditate any other way.
Cheap, low-tech stress relief may also protect against depression, insomnia, and anxiety
Meditation is no longer just for the groovy folk. A just published study in the American Journal of Hypertension suggests the practice may bring cardiovascular and mental-health benefits. The research, conducted at American University in Washington, followed 298 students, half of whom practiced transcendentalmeditation for 20 minutes once or twice daily over three months and half of whom did not. Results: A subgroup of subjects in the meditation group who were at increased risk for hypertension significantly lowered their blood pressure and psychological distress and also bolstered their coping ability. The average reduction in blood pressure in this group—a 6.3-mm Hg decrease in the top (systolic) number of a blood pressure reading and a 4-mm Hg decrease in the lower (diastolic) number, compared with the control group—was associated with a 52 percent reduction in the risk of developing hypertension in the future. Meditators who were not at increased risk for hypertension saw a reduction in psychological distress, depression, and anxiety as well as increased coping ability but no significant lowering of blood pressure. The results are particularly meaningful at a time when “improvement in mental health is of great concern as greater numbers of college students are being treated for anxiety and depression than ever before,” says lead study author, Sanford Nidich, professor of physiology and health at the Institute for Natural Medicine and Prevention at Maharishi University of Management in Iowa.
Lately, meditation has been garnering attention from a host of medical and scientific researchers. More than 120 meditation studies are listed on clinicaltrials.gov, a clearinghouse for research supported by the National Institutes of Health, investigating the intervention in patients with conditions from cancer and heart disease to post-traumatic stress disorder, insomnia, and binge eating. It’s no cure-all, but early research is suggesting meditation could play a helpful role in mediating the stress response that contributes to a number of physical and mental conditions.
In a country famous for medical innovation and high-tech treatments—not to mention their high cost—Americans, too, have begun to embrace complementary and alternative interventions like meditation, acupuncture, and “natural” supplements. According to a recent study sponsored by the NIH’s National Center for Complementary and Alternative Medicine, more than 1 in 3 adults sought such healthcare in 2007—and collectively spent $40 billion out of pocket. But with the exception of the classes, books, or CDs one might buy to learn the ins and outs of “om,” focusing on one’s breath, or becoming more mindful, the practice of meditation is free.
One simple thing seems clear: Find a type of meditation that you like. “What’s really important,” says Richard Davidson, neuroscience and meditation researcher at the University of Wisconsin-Madison,” is that a person find a particular style [of meditation] they’re comfortable with so they continue to practice.” Some styles train practitioners to focus on an object or a mantra; others cultivate positive emotions; others still aim to train practitioners not to judge thoughts that arise but to just accept them and not get attached. More meditation, it seems, offers stronger effects; Davidson’s research on monks who had practiced for tens of thousands of hours in their lifetimes managed to change their brains’ functioning and structure. Benefits appear to be attainable with less of a time commitment, he adds—perhaps somewhere between 20 and 40 minutes daily.

Meditation Pose
Not all doctors have bought into the merits of meditation as a treatment, nor should they just yet. The hard research medical practitioners swear by is still in the early stages. The National Center for Complementary and Alternative Medicine is starting to fund needed research with larger sample sizes of participants and solid study design, says Jeffrey Greeson, meditation researcher and assistant clinical professor in the department of psychiatry and behavioral sciences at Duke University School of Medicine. He predicts that results will begin to emerge in the next five years. Meantime, based on some encouraging preliminary findings, here are five reasons a clinician hip to the importance of the mind-body connection may cite for prescribing meditation—and one reason she may choose not to.
By SARAH BALDAUF for US News
Now & Zen – The Meditation Timer Store
1638 Pearl Street
Boulder, CO 80302
(800) 779-6383
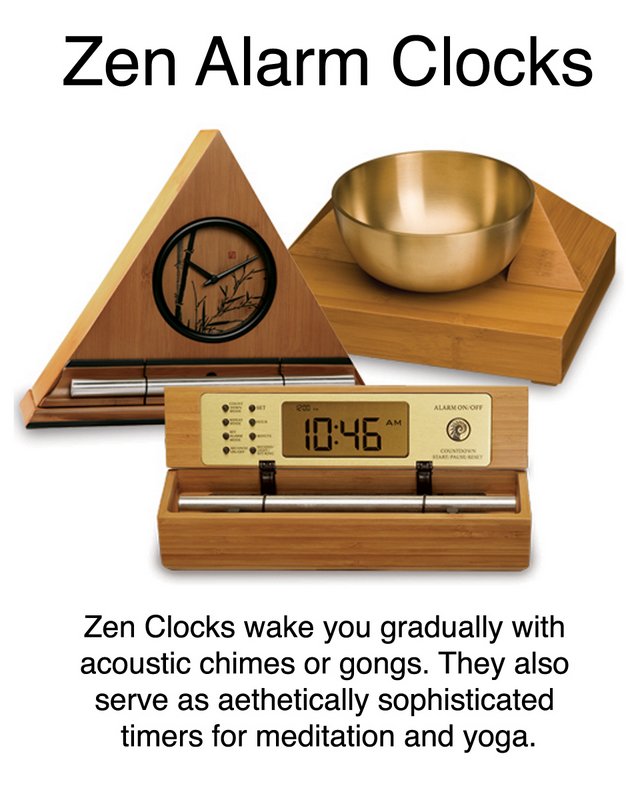
Posted in Meditation Tools